Klf4-dependent pivotal role of smooth muscle-derived Gli1+ lineage progenitor cells in lung cancer progression
Klf4-dependent pivotal role of smooth muscle-derived Gli1+ lineage progenitor cells in lung cancer progression
Lu, S.; Navarro, A. C.; Johnson, A. M.; Noble, T.; Jolly, A. J.; Moulton, K. S.; Nemenoff, R. A.; Weiser-Evans, M. C.
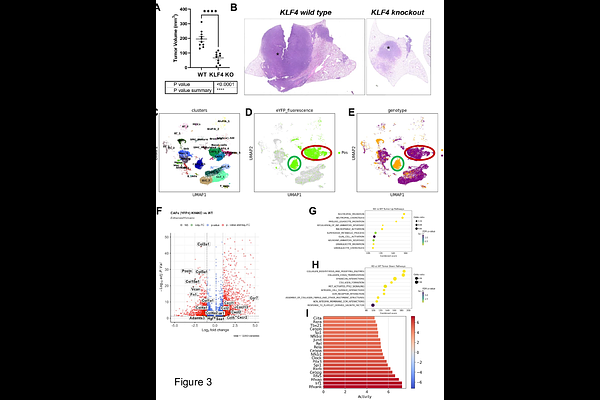
AbstractLung cancer remains the leading cause of cancer-related deaths worldwide. Despite the remarkable efficacy of immune checkpoint inhibitors, only a subset of lung adenocarcinoma (LUAD) patients respond and many eventually progress, underscoring the need to develop novel combination therapies. The interaction between cancer cells and the tumor microenvironment (TME), a complex niche including cells of the innate and adaptive immune system, cancer-associated fibroblasts (CAFs), vascular cells, and extracellular matrix (ECM) plays a vital role in tumorigenesis and cancer progression. Using fate mapping, we previously identified a novel subpopulation of resident vascular stem cells derived from vascular smooth muscle cells, designated AdvSca1-SM (vascular Adventitial location, Stem cell antigen-1 expression, SMooth muscle origin) cells. AdvSca1-SM cells are the predominant cell type responding to vessel wall dysfunction and their selective differentiation to myofibroblasts promotes vascular fibrosis. SMC-to-AdvSca1-SM cell reprogramming is dependent on SMC induction of the transcription factor KLF4, and KLF4 is essential for maintenance of the stem cell phenotype. The function of AdvSca1-SM cells in LUAD tumorigenesis has not been explored. Using an orthotopic immunocompetent mouse model of LUAD, we demonstrate that AdvSca1-SM cells are a major component of lung tumors, significantly contributing to cancer associated fibroblasts (CAFs). Compared to AdvSca1-SM cells, CAFs have altered ECM gene expression with a reduction of a stemness signature. AdvSca1-SM-specific genetic ablation of Klf4 altered their phenotype resulting in inhibition of communication between cancer cells and CAFs, decreases in innate immunosuppressive populations, and increased T cell infiltration into the tumor. Targeting this population may represent a novel strategy to improve the response to immunotherapy.