Lymphatic dissemination drives systemic invasion by diverse clinically relevant extracellular bacterial pathogens
Lymphatic dissemination drives systemic invasion by diverse clinically relevant extracellular bacterial pathogens
Siggins, M. K.; Kwong Li, H.; Huse, K. K.; Pearson, M.; Openshaw, P. J.; Jackson, D. G.; Sriskandan, S.
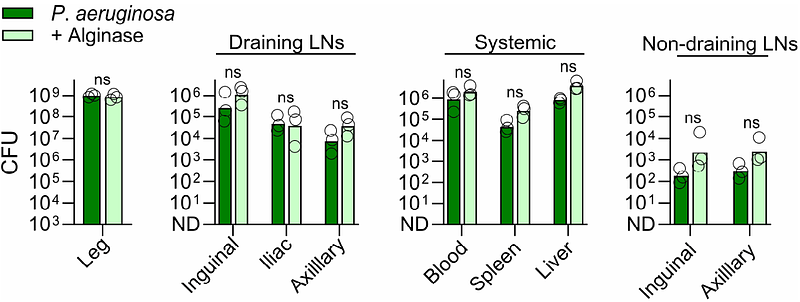
AbstractSystemic bacterial infection is typically attributed to direct blood vessel invasion or intracellular transit, while the role of the lymphatic system remains largely unexplored. We previously showed that Streptococcus pyogenes disseminates extracellularly via the lymphatics. Here, we extend this observation to a diverse group of important extracellular bacterial pathogens, including Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Staphylococcus aureus, and Streptococcus agalactiae. In a murine soft tissue infection model, nearly all clinical isolates reached both local and distant draining lymph nodes and systemic organs, with minimal bacterial presence in non-draining nodes. This pattern demonstrates that diverse bacteria can traverse filtering lymph nodes and supports lymphatic rather than haematogenous spread as the primary driver of systemic invasion. Bacterial dissemination varied between species and among isolates of the same species, with capsular polysaccharides emerging as one key determinant. These findings establish lymphatic metastasis as a common but under-recognised route of bacterial invasion, with implications for pathogenesis, immunity, and treatment.